Root Cause: Understanding the ‘Why’ Behind Behavioral Health
This article appeared in the Vail Daily on October 20, 2020 and first appeared in Vail Health Magazine, which is produced in partnership with Colorado Mountain News Media. Pick up a copy for free at locations around the valley or go to vailhealthmagazine.org to read the digital version.

What makes someone healthy? Is it the numbers measured in blood pressure, heart rate, cholesterol and body weight? Or is it the wellbeing of the body, mind and spirit?
Increasingly, patients are seeking treatment for conditions related to behavioral health — issues that can include depression or anxiety, weight loss or diabetes management, and quitting smoking, drinking or drugs. As a result, health care is moving beyond the numbers, and integrated behavioral health care is becoming the gold standard.
Mental health is a key component in this puzzle. Though we all have “down days” or “feel blue” now and then, some people experience persistent, debilitating and devastating depression, anxiety or mental illness.
While there isn’t one reason why people experience metal health challenges, most can be traced back to a combination of factors, both biological and environmental, including genetics and biology, life experiences and external factors. However, by understanding the causes, behavioral health care providers can work to unlock the right treatment, or combination of treatments, for each person.
How Genes Can Impact Mental Health
Does mental illness run in families?
Is there a gene that determines whether or not an individual will suffer from mental health problems?
Yes and no.
“Even though we have lots of research on the root causes of mental illness, whether it’s depression or anxiety, for instance, it’s almost impossible to link it to one thing,” explains Dr. Casey Wolfington, licensed psychologist and community behavioral health director for Eagle Valley Behavioral Health (EVBH). “We’re such complex creatures and so much of who we are is a combination of both our genetics and what we experience as humans.”
Genes may play some part in mental health disorders, but it’s not as straightforward. Instead, mental health disorders like depression and anxiety are what Dr. Marshall Thomas, director of the Johnson Depression Center at the University of Colorado and the medical advisor to EVBH, calls a polygenic disorder: There are multiple effects based on multiple genes. To add to the mix, there’s also a gene environment interaction that doctors believe starts even before you’re born — a mother’s stress hormones can actually trigger certain things in a baby’s genes prenatally.
“Your genes aren’t static. They’re turned on and turned off by the environment, especially by trauma and stress,” Dr. Thomas explains. “So there’s a huge role that the environment plays on who ends up depressed, who ends up with certain chronic diseases.”
In other words, there may be genes that indicate mental health issues like depression, bipolar disorder or schizophrenia, but just because those genes exist doesn’t mean that those illnesses will manifest.
There is also some indication that families can have a predisposition for certain mental illnesses, like depression or bipolar disorder.
“For example, with depression, if you have a first-degree relative (like a mother or sibling) with major depression, you’ve got a 10% chance of having major depression yourself,” Dr. Thomas says. “It’s not 100%, it’s 10%. If you look at the general population, that’s probably 5%. So that genetic predisposition puts you at increased risk.”
As a result, the ability to reduce or alleviate stressors in the environment can play a major factor in preventing depression, or mitigating the effects of depression, if you’re genetically predisposed to the condition.
“If you take appropriate care and practices to help mitigate environmental stressors like early loss and trauma, you’re less likely to actually manifest depression,” Dr. Thomas says.
This is positive news. Just because there are genetic indicators or family history, experiencing a mental health challenge is not a foregone conclusion. Instead, our environment and our connections to other people can not only make a difference in our own lives, but we can make a difference in other people’s lives.
“That should be where a lot of our attention is: How do you get upstream with this and create nurturing environments either in the family or in the community that mitigate stress in kids and help them not walk into adolescence or adulthood with a body that’s already had all the stress genes turned on to set them up for anxiety and depression and substance abuse?” Dr. Thomas questions.
Nurture Versus Nature
These environmental stressors — everything from loss to trauma and abuse — can play a huge role in behavioral health.
“There are studies where they count how many adverse childhood events someone has,” Dr. Thomas says. “And the research shows there’s a direct correlation between the high number of adverse events that happened in childhood and the instances of medical illness and psychiatric instances.”
As a result, creating nurturing and supportive environments, both in the home and in the community, is crucial for creating positive behavioral health. This is where the importance of relationships comes in.
Research has linked the number of connections that one person has to his/her resilience and ability to overcome difficult times or obstacles in life. This goes beyond the early years. In addition to having strong relationships at home, it’s important to have other connections — at school, in the workplace and in your social life. Your support group doesn’t only help when uncontrollable situations occur, but it can also create positive influences throughout life.
“Even if genetics show a predisposition for anxiety or depression or learning disabilities, for instance, our social connections and strong relationships with other people are our biggest predictors of health,” Dr. Wolfington says.
The Biological, Psychological and Social
When it comes to treating behavioral health issues, it’s important to look at all aspects that could be contributing to the problem.
“When we’re talking about mental health, oftentimes we’re thinking about specific diagnoses rather than all of the different systems that contribute,” Dr. Wolfington says.
For example, someone with diabetes may also be experiencing anxiety or depression. Instead of treating the depression as a separate, individual illness, the patient may see a better outcome if the mental aspect of dealing with the diabetes is addressed. Having tools and strategies to deal with the mental burden can ease the depression, leading to improved mental health and, hopefully, better management of blood sugar.
In short, everything is connected and dealing with just one aspect of a person’s condition limits overall wellness.
“In order for us to enhance behavioral health or physical health, we have to look at all dynamics of health,” Dr. Wolfington explains.
Tapping Into Genes for Treatment
Pharmaceuticals are often part of a treatment plan for mental illnesses. But what if there was a way to use your genes to create a more effective treatment? This is a question many pharmaceutical companies are trying to answer. Genes may determine some of our responses to treatment, but again, it’s not a question of addressing a single gene. And though several companies tout genetic testing as a means to guide choices for antidepressants, “experts with no financial interest in genetic testing have repeatedly recommended that genetic tests should not be used in choosing treatments for depression,” wrote Dr. Bruce Cohen and Dr. George Zubenko on the Harvard Health Blog.
In fact, the FDA advised that the tests had no proven value and should not be used. The organization also stated that the use of the tests could lead to inappropriate treatment choices that might harm patients.
“So instead of getting overly focused on genetic testing, I think the focus should be on comprehensive care that is guideline-based. Comprehensive care is care that deals with and understands the biology, the psychology and the social aspects of the mood disorder the person has,” Dr. Thomas says. “At this point I would reserve genetic testing for people where a comprehensive stepped-care approach and multiple medication trials have not been successful.”
Expanding and Improving the Quality of Care
Regardless of whether or not behavioral health is linked to biology or environment, having access to care can directly improve mental health.
“Not having access to appropriate medical care or health insurance has been consistently linked to poor behavioral health and physical health outcomes,” says Dr. Wolfington. “That is one of the reasons that Vail Health felt it was so important to create an integrated behavioral health environment within our Colorado Mountain Medical clinics.”
One challenge that both rural and mountain communities face is creating better access to ongoing care. This manifests not only in affordability and access for patients, but also having the behavioral health professionals available to help. Until recently, there were no training opportunities for prospective psychologists or clinicians in the mountains.
However, in 2014, Bright Future Foundation, a community fundraising partner of EVBH, created the Colorado Psychology Internship Consortium, also known as CO-PIC, which prepares interns to meet the needs of rural and underserved populations.
“It’s a really big deal because the vast majority of people who are in practice as psychologists, doctors or physicians typically practice in close proximity to where they finished their residency,” says Dr. Wolfington, who helped establish CO-PIC. “The lack of pre- and post-degree training opportunities is one of the reasons that Eagle County struggled to effectively recruit providers.”
Eagle Valley Behavioral Health has now been established as part of CO-PIC, creating partnerships with prospective psychologists and clinicians from schools like the University of Denver to try and create a pathway for the behavioral health workforce in our community.
“Without a formal pathway, we’re just relying on clinicians with high student loan debt to take the risk of moving to our high cost of living, low housing availability community, and it’s not going to happen,” Dr. Wolfington says. “We have to be really intentional in making these partnerships. Otherwise, we’re always going to have a behavioral health provider workforce shortage.”
By increasing access to care, which includes both mental and physical care, the community as a whole will be healthier.
Mood and anxiety disorders are not like a virus — treating them is not a “one and done” situation, Dr. Thomas says. Instead, they require ongoing interventions, including lifestyle interventions, psychological interventions and sometimes biological interventions. The earlier you intervene, the better the outcome.
Approaching behavioral health with a wholistic approach early on helps mitigate the unavoidable life stressors and trauma that can lead to mental health issues. So don’t ignore your behavioral health — it’s just as important as those other numbers on the doctor’s chart.
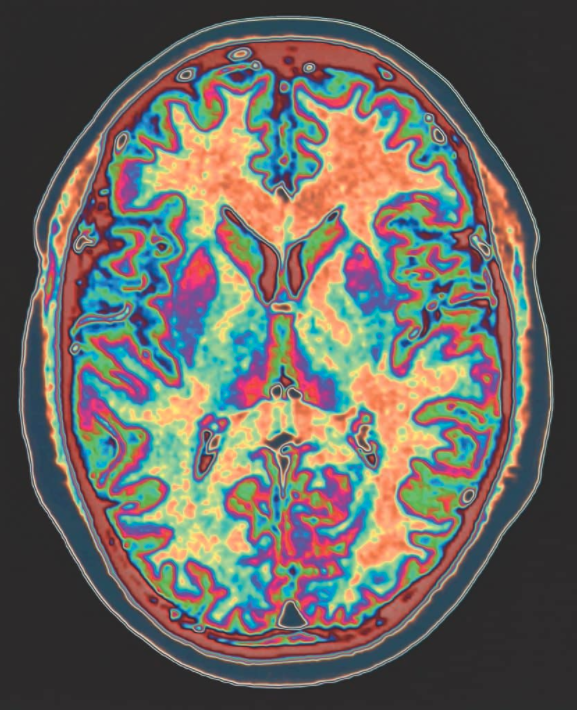
Research shows that living with anxiety actually changes the brain.
Even if genetics show a predisposition for anxiety or depression or learning disabilities, for instance, our social connections and strong relationships with other people are our biggest predictors of health.


